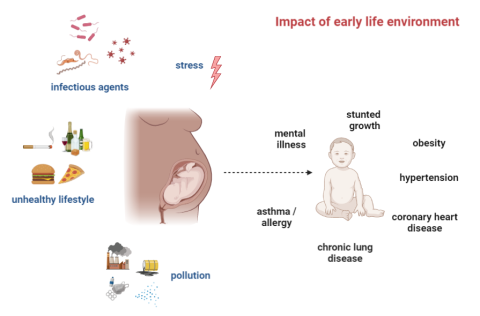



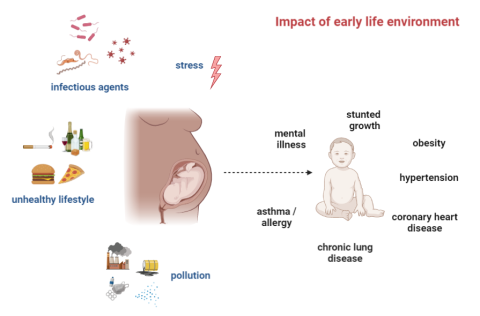
Maternal infection and other environmental disturbances in early life can play a decisive role educating the growing immune system. Recent evidence shows that changes affecting pregnancy can tip the balance in determining the likelihood of inflammatory disorders, and can affect immune responses into adulthood. The first “1000 days” in humans have been designated as a pivotal “window of opportunity” for effecting profound change for the development of bodily systems, including appropriate immune functioning with lasting effects throughout lifetime.
What is fetomaternal Immunology?
In our work, we explore the origins of non-communicable diseases (such as inflammatory conditions), and compare these to healthy maturation of the growing immune system. We engage in basic, pre-clinical investigation of the processes involved in healthy and in altered pregnancies, including maternal infection during gestation, to observe what effects diverse stimuli can have on shifting immunological priming and disease outcomes. Through fieldwork in regions endemic for significant Neglected Tropical Diseases, we address the particular concerns of how these under-examined infectious diseases can impact women’s health, especially during the prenatal period and childbirth. We apply state-of-the-art immune phenotyping to profile changes to neonatal development and uncover the mechanisms driving these changes through pre-clinical modelling. Our aim is to deliver improvements to ensure healthy pregnancy outcomes in diverse settings, and strengthening the link between events at these key time points for healthier outcomes for the future.
Why is maternal health such a core aspect of global health in the 21st century?
Safeguarding maternal health during pregnancy is a fundamental pillar of improving the health of humans globally. It is in this impressionable early period of life, along with the transitional period into motherhood, where the effects of modernization and urbanization are felt most acutely. Across the globe, the appearance of novel infectious agents, the persistence of familiar ones, increasing awareness of maternal diet and microbiomes, and inflammatory triggers, against the backdrop of rapid urbanization present renewed challenges with changes to the traditional approach to pregnancy and childbirth. Maternal infections or stress can interfere with the immune processes involved in many clinically relevant areas, which range from inflammatory diseases and immune disorders, early development, vaccines and management of co-infections to successful development following healthy pregnancy. As such, a deeper investigation of how these microbial exposures and infectious challenges modulate immune memory in a more global sense will enrich our understanding of immune interactions with the environment; and provide tools for fine tuning immune responses and modulation of immune disorders. Such considerations may affect interventions regarding infection, including treatment of chronic infections, and for immunization during and after pregnancy (including during the nursing period). To enhance the translational aspect of this research, we organize activities with the Center for Global Health (CGH), such as a workshop on women's health in Gabon, to engage stakeholders, which is imperative not only for the formulation of recommendations and policies, but also for acceptance within affected communities.
What is the concept of “Developmental Origins of Health and Disease”?
With the rapid changes to our living conditions over the last century, the impact of the environment on human health has become increasingly apparent. We are beginning to understand that perturbations to the developmental environment in early life can drive immunological imprinting, with the origins of some diseases linked to permanent changes effected in utero, sparking a dialogue about the fetal origins of adult disease. More recently, environmental factors such as maternal infection status have been observed to play a role in modulating future inflammatory outcomes. These are relevant for allergic and immune heterogeneity, such as infectious disease outcomes or vaccination strategies in endemic areas. As the focus shifts towards personalizing aspects of population health, which includes considering individual history in understanding the effects of past and current microbial and parasitic exposures, the needs of vulnerable communities, and the dysregulated states that arise in the urbanized settings, will change the interpretations of the differences between populations and inform customized approaches to address their needs.
What are your latest findings on the impact of maternal shistosomiasis?
Parasitic diseases have been common throughout human history, and fall into the category of infections with changing incidence due to increased hygiene and urbanization. Immune processes involved in allergy form part of the type 2 immunity also involved in protecting against toxins and parasites, with parasites, including schistosomes, noted for their ability to downmodulate these immune responses to ensure their survival in hosts. Almost 40 million women of childbearing age are estimated to be infected with schistosomes, representing a significant disease burden, which potentially impacts the likelihood of a successful pregnancy for many of these women; along with a board chance for fetomaternal crosstalk, which could be impacted by the presence of these infections. Our previous studies have shown modified inflammatory outcomes in the circulation and placentas of these infected women and within our new consortium “HelmVit”, we strive to deepen our understanding of such infection-derived disruptions of the immunological crosstalk. Together with partners from Gabon and Benin in Africa, we investigate in large mother-child cohorts. Our pre-clinical work indicates that maternal infection influences not only predisposition towards allergy in offspring, but also drives widespread priming across immune cell subsets that we will continue to explore in detail, particularly in the context of trained immunity in these models as well as in human cohorts.
Current projects in Fetomaternal Immunology and DOHaD:
- Treatment of helminth infection during pregnancy and its effects on antigen-specific immune responses and disease development in offspring
- Innate training in the context of transmaternal helminth infection
- Persistent immune priming via maternal inflammation
- Regional and infection-specific effects on Vitamin D and immune parameters at birth and their connection to allergic disease
- The role of maternal cytokines during gestation as a factor in future immune responses